Telehealth as a practice has been around for half a century. But its popularity and importance surged in the later 2010s and then nearly doubled due to the pandemic. Does the current state of technological progress indeed allows the provision of effective remote healthcare services? Are virtual appointments as effective as in-person visits? What does the future of telehealth hold for the patients and services providers? Let’s get you answers to these questions and more!
What is Telehealth?
The World Healthcare Organization (WHO) defines healthcare as the “delivery of health care services, where patients and providers are separated by distance.”
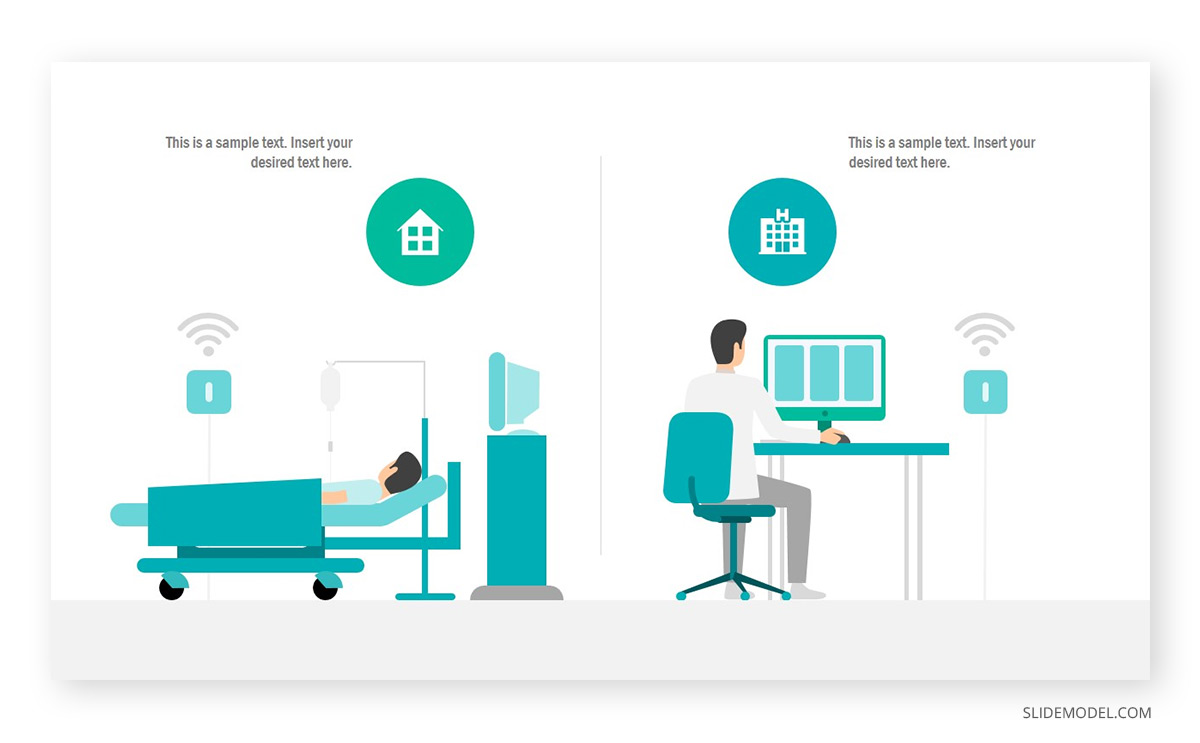
Thanks to high-speed Internet, virtual conferencing tools, and 4G (and soon 5G) connectivity, healthcare professionals can perform remote diagnostics and provide virtual healthcare services to patients who cannot (or do not wish to) travel to the nearest hospital location. Originally launched as an initiative to serve the elderly, vulnerable groups, and patients living in remote locations, telehealth services have entered the mainstream in 2020.
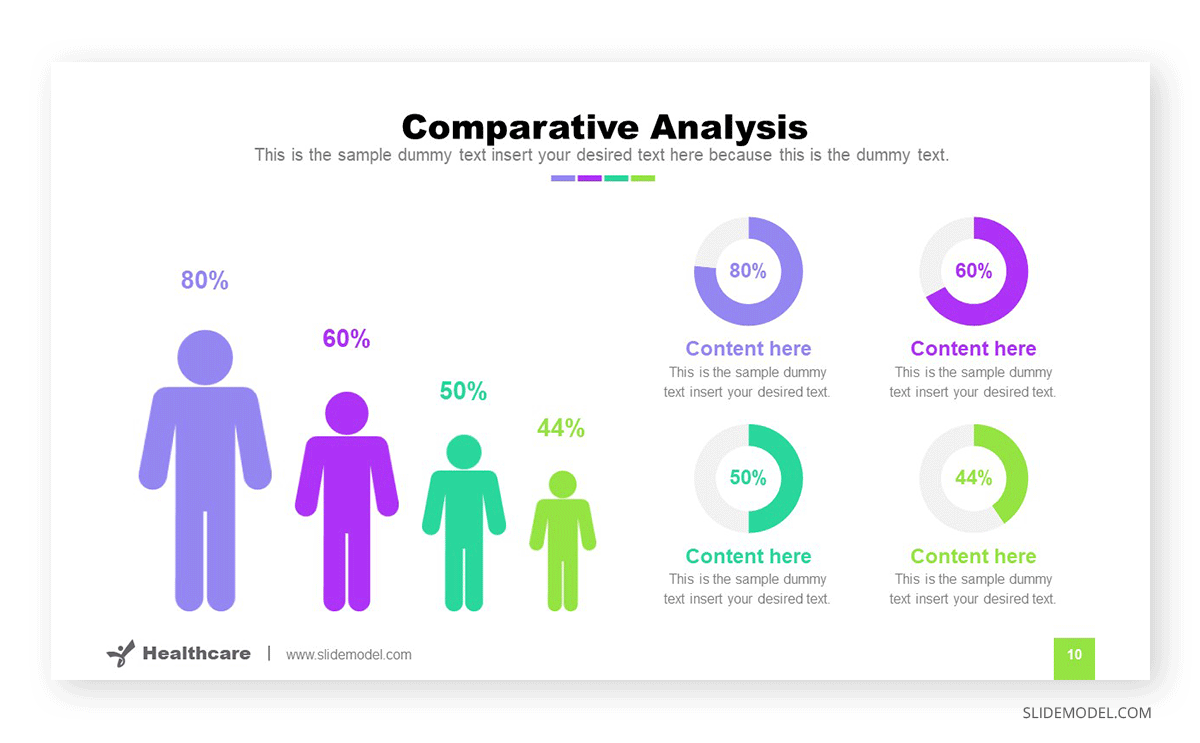
Before the pandemic, one-quarter of patients weren’t interested in trying a telemedicine app. However, many were prompted to use remote healthcare services during the outbreak. Then they realized that such virtual appointments don’t differ much from in-person visits. The newly found affinity for telehealth further translates to higher adoption levels. After the pandemic resolves, 83% still see themselves using telehealth services for patients.
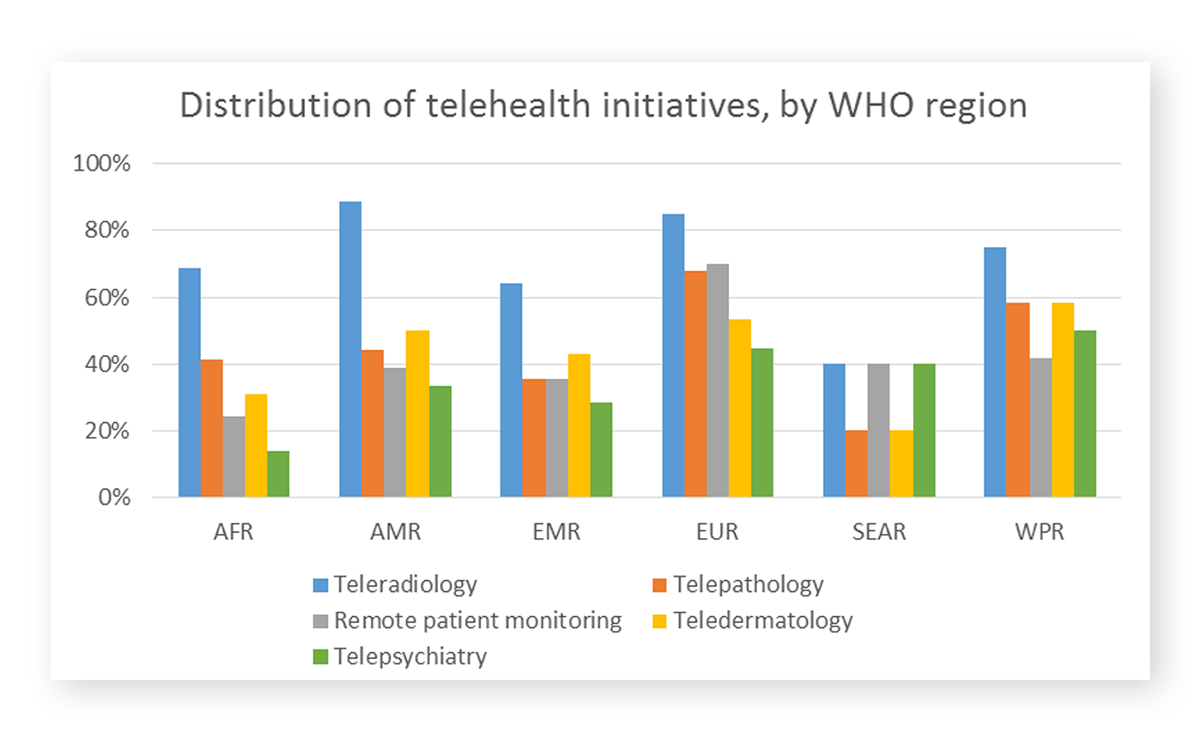
Globally, legislators are also en route to adopting new telehealth technology. Per WHO, over 50% of member states already have a national telehealth policy in place. Many also plan to further expand the scope of provided services:
Telehealth vs Telemedicine: What’s the Difference
Telemedicine is another term, used frequently along or instead of “telehealth”. However, there’s an important difference between the two of them.
According to the AAPF foundation, telemedicine is a medical practice of using telecom infrastructure to deliver remote care to a patient.
Telehealth, on the other hand, refers to the underlying technology in healthcare (software, telecom, and connectivity infrastructure) that’s required to provide care and medical services remotely.
Contrary to telemedicine, telehealth encompasses a wider range of services than telemedicine. Telemedicine refers to clinical remote services, whilst telehealth refers to non-clinical remote services.
A Brief History of Telehealth
Telehealth as a concept emerged at the dawn of the 20th century.
Willem Einthoven, the inventor of the electrocardiogram was among the first scientists to propose a concept of remote service delivery. In 1906, he published a paper, detailing how a telecardiogram might work.
In 1925, the medical community speculated how telemedicine companies of the future might look like. The cover of the Science and Invention magazine featured a doctor using the radio and a prototype device for remote video examination.
By-mid century, telehealth started getting closer to the earlier envisioned reality. In 1948, doctors sent radiological images via the telephone for the first time. In the 1960s, Nebraska Psychiatry Institute started using closed-circuit TV for performing remote psychiatric consultations.
Finally, in 1993, the American Telehealth Association was founded and many of today’s telehealth and telemedicine practices were standardized.
But of course, the boom of telehealth happens in the 21st century. Internet connectivity has become ubiquitous and low-latency, allowing it to transmit large volumes of data in near real-time. So that doctors could exchange more advanced imagery and high-def video to perform diagnosis.
What are the telehealth services, available to patients today? Here are some:
- Patient portals
- Online doctor consultations
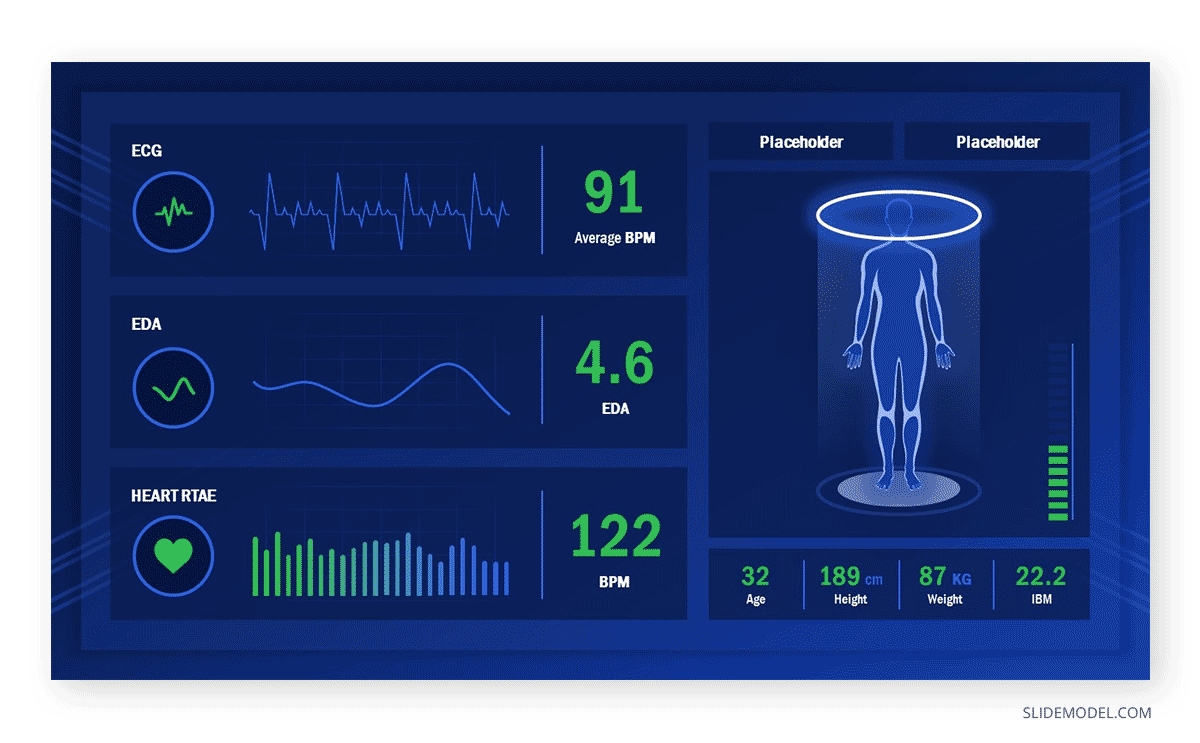
- Remote vitals monitoring
- EMR/EHR systems
- Medical wearables
That’s just the culprit though. The global telemedicine market is projected to grow at an annual CAGR of 23.5% and reach $185 billion by 2026. So there’s surely going to be even more innovative patient services and telehealth companies, entering the market.
The Benefits of Telehealth
According to McKinsey, over $250 billion of current US healthcare spend could potentially move to virtual providers over the next years. That’s a good thing for healthcare services providers since telehealth enables the following benefits:
- Access to care for patients: Virtual urgent care as an alternative ER visits. Plus, the option is easier for patients with limited mobility, the elderly, and those living in remote locations. During the pandemic, virtual appointments also help minimize potential exposure to the virus.
- Faster access to regular check-ups: When done online, regular checkups help both the doctor and the patient save time. Currently, patients spend ~45 minutes traveling to and waiting for their medical appointments on average and then 75 minutes with their doctors. Virtual visits can cut that time in two. Such an option is particularly necessary for people with chronic conditions who require regular visits.
- Lower service costs: Telemedicine reduces the overheads of providing care. According to the American Journal of Emergency Medicine, the net cost savings per telemedicine visit is around $19-$121 depending on the visit type. Telemedicine is good for the patients’ wallets too. The average cost of a teleconsultation is $38 versus $114 for a face-to-face meeting.
- Innovative care: IoT sensors and remote healthcare applications can usher in a new era of healthcare. Already, patients can receive timely medicine administration at home via medical gadgets that can automatically disperse injectable drugs and send vitals to the healthcare provider. Zoom telehealth services have become very popular too. Meaning that patients can easily schedule visits with an array of specialists — from a dermatologist to a speech pathologist.
Popular Telehealth Services
Today patients can access a broad range of telehealth services, provided both by the national healthcare systems and private telehealth companies. These include:
Teleradiology: Teleradiology was among the first telemedicine services to be ever delivered. The film used to be scanned through a digitizer. But nowadays the images are read directly on a computer, allowing images to be viewed anywhere in the world overnight.
Telepharmacy: Doctors can now enter electronic orders for drugs, review them remotely, and even dispense medicine remotely. With the help of video conferencing, the entire pharmacy experience can be done remotely. That leads to some solid benefits for the patients and healthcare providers. One study found that a remote pharmacy saved cancer patients over 27,000 miles of travel. Another research paper notes that telepharmacy managed to weed out and rectify mistakes in medication among 19% of referred patients.
Online therapy: Telehealth counseling services have gained a surge in popularity during the pandemic. The mentally taxing times made a lot of us seek solace and professional help. Thankfully, we could conveniently access it online. Telehealth commoditizes access to therapy and enables more people to get timely help. A 2017 study found that over 46.6 million Americans suffer from mental health issues. Yet only 42% actually received treatment. Telehealth services could help bridge this gap.
Telehealth physical therapy: Physical therapy (PT) is a proven method to accelerate recovery after surgeries and major traumas. However, access to such services can be challenging for people with limited mobility or those in remote locations. The new generation of remote physical therapy devices such as the Virtual Exercise Rehabilitation Assistant (VERA) system (powered by sensors and 3D simulations) could help such patients get access to care too. According to the Journal of Bone & Joint Surgery, virtual PT patients who practiced with a system and received weekly telehealth visits were hospitalized less and were more physically active than a patient group who used traditional PT.
The Future of Telehealth
Major transformations are underway in the healthcare sector. In particular, the combination of cloud, AI, and IoT technologies holds great promise for further transforming the face of modern healthcare.
According to Tata Consultancy Services, among 56 leading healthcare organizations, 86% already use AI at some capacity and spent $54 million on average on this technology stack. How is AI used in healthcare today? In several ways:
- Clinicians leverage Google’s machine learning algorithms to remotely diagnose and treat diabetic retinopathy.
- State-of-the-art deep learning algorithms also facilitate doctors with diagnosing breast cancer and doing so at a higher rate than 11 human pathologists.
- AI also facilitates drug discovery. One company used AI algorithms to synthesize a rheumatoid arthritis drug that has also proven to be effective for treating Covid-19.
In the future, machine learning and deep learning algorithms, trained on a wider range of clinical data, could become capable of performing even more complex medical procedures both in hospitals and remotely.
For example, radiology and cardiology departments could fully rely on artificial intelligence for analyzing test results, X-rays, CT scans, and other diagnostics tasks. While the algorithms handle the mundane tasks, human doctors could handle complex and emergency cases where manual tasks need supervision.
In terms of telehealth, service providers could improve the levels of remote medical care tremendously with better computer vision technologies. For example, at-home patients could agree to have a video monitoring device installed that would monitor if they are taking their medication and doing other exercises properly via image recognition technology. Doctors then could receive, a quick summary of the patient’s activity and performance and provide them with updated recommendations.
AI also has a strong potential to transform how primary care is provided. With the improvements in Natural Language Processing (NLP) technology, AI algorithms could take over the data collection tasks during telemedicine visits. Instead of conversing with a human, patients would tell their symptoms to a human-like avatar, asking them standard questions about their symptoms and taking other measures remotely such as temperature, pulse, and other vitals via remote sensors.